In medical education, the transition from theoretical knowledge to clinical practice is often a complex and challenging process. As an advanced teaching tool, whether the brain-attached cerebral artery and neural model can effectively help medical students shorten this transition period has become the focus of attention of many educators and clinicians. By providing accurate anatomical, pathological and operational simulations, the model is considered an important means to improve the efficiency of medical education and clinical competence. This paper will explore how this model works in teaching and practice, and its potential to accelerate the learning process.
1. Help students better understand neuroanatomy
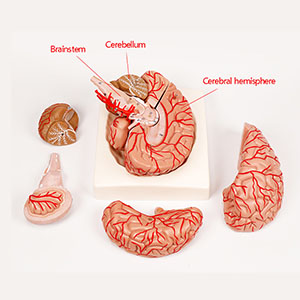
The Cerebral Appendicular artery and Neural model provides a highly simulated anatomy of the nervous system, which not only shows the major vascular networks and neural connections of the brain, but also simulates the lesions that may be encountered. Through such realistic and detailed models, students can clearly see the complex structure of the brain and how these structures are related to each other. Compared with the traditional two-dimensional map or virtual reality technology, this three-dimensional model can help students master the spatial structure and improve their understanding ability.
Studies have shown that students are more likely to form deep impressions when confronted with real three-dimensional models than when learning through traditional textbooks. Through intuitive observation and manipulation, students are able to understand the complexities of neuroanatomy in a short period of time, thus laying the foundation for subsequent clinical practice. This model can help students establish correct spatial cognition at an early stage, and be able to transfer theoretical knowledge to clinical application in a short time.
2. Simulate clinical operation to improve practical ability

The brain attached cerebral artery and neural model are not only used for anatomical learning, but also for simulating complex clinical operations such as neurosurgery, vascular repair, etc. Through the practical operation of these models, students can practice difficult operations such as cerebrovascular angiography and brain tissue excision, and directly experience operational difficulties in clinical Settings. Different from traditional paper learning, students can immediately apply theoretical learning to practical operation through this interactive learning, reducing the situation that they may encounter in clinical practice is not skilled or wrong judgment.
According to some educational studies, students trained using simulation models are often able to acquire the necessary skills in a relatively short time when performing actual clinical operations. For example, when performing brain surgery, students are able to gradually improve the accuracy and confidence of the surgery by repeatedly practicing the operations in the model. This practical simulation not only enhances the students' clinical ability, but also shortens the transition period from theory to practice.
3. Accelerate the development of clinical skills

The use of the cerebral artery and neural model is not limited to the teaching stage, it can also help medical students master key clinical judgment and operational skills before entering the clinical environment. Traditional teaching methods often focus on theoretical learning, often neglect the cultivation of students' practical ability. However, the introduction of this model can build a bridge between theoretical learning and practical clinical practice, so that students can deeply understand the practical application of theoretical knowledge in the process of hands-on operation.
For example, students can simulate cerebrovascular therapy by operating models, and can better understand the relationship between vascular structure and surrounding tissues, thereby reducing the misoperation and risk caused by lack of experience in actual operation. This process can greatly shorten the adaptation period of students from the classroom to the clinic, so that they can adapt to the clinical environment more quickly, reducing the risk of unskilled operation.
4. Data support: Improve teaching efficiency and clinical results
According to the relevant data, students trained with the model of the cerebral appendicular arteries and nerves showed significant improvements in actual clinical manifestations. Studies have shown that the success rate of clinical procedures among participants trained with the model is about 20 to 30 percent higher than those who do not use the model. In addition, after receiving simulation training, the students were able to identify the symptoms and abnormal signals of common brain lesions more quickly, improving the accuracy of diagnosis.
This simulation training method not only improves the operational accuracy of students, but also reduces the error rate in the course of clinical practice. The students' coping ability in practical clinical work has been significantly improved, especially the decision-making ability and operation speed in emergency situations have been strengthened. This shows that simulation training not only contributes to the application of theoretical knowledge, but also promotes the rapid improvement of students' clinical skills.
5. Conclusion
Overall, the introduction of the brain-on-brain artery and neural model undoubtedly provides great value to medical education. It helps students better understand complex neuroanatomy by providing realistic, detailed structures of the nervous system, and quickly gain experience in practical operation. This model can not only accelerate the transition of students from theoretical learning to clinical practice, but also improve the accuracy of clinical skills and decision-making ability to a certain extent, so as to effectively shorten the learning cycle and improve the overall teaching effect. Therefore, as an important tool in medical education, cerebral artery and neural model have a position that cannot be ignored in modern medical training.
